Ben Behind His Voices Blog
One Family’s Journey from the Chaos of Schizophrenia to Hope
NEW in 2022! – the Ben Behind His Voices audiobook has been updated with a new intro, epilogue, and bonus material! – available only in audiobook form.
Hear all of the original award-nominated memoir, and find out what has happened in the decade since. We continue our journey into hope.
Not-So-Happy Holidays? How to Manage with SMI in the Family
What if, for families coping with SMI (serious mental illness) in a loved one, the holiday season is "the most difficult time of the year"?
The 3 Moms Discuss - Holidays past, in joy, crisis or grief - and how we currently celebrate what is...the best we can.
Some tips we share:
Lower Holiday expectations and Marketing Myths (e.g., perfect holidays)
Plan Ahead - even for possible disaster
Have a Plan B - and maybe C, D...
Include Your Loved One as Much as Possible, Especially if They Can Help
Don't Let the "Unsqueaky Wheels" feel ignored
Cherish the Good Moments - Find the Positives
Be Willing to Change Traditions as Needed
Set and Enforce Limits - Know Your Boundaries
Imagine How it Is for Your Loved One
Family Love Matters - You Do Make a Difference
Happy (and Realistic) Holidays to You All!
Want to Share Your Story in a Voice message?
Resources:
Look Again Podcast: https://www.bcss.org/lookagain/
Tips from NAMI: https://www.nami.org/Blogs/From-the-CEO/December-2021/The-Most-Difficult-Time-of-The-Year-Mental-Health-During-the-Holidays
Mindy and her book: https://mindygreiling.com/
Randye and her book: https://benbehindhisvoices.com/
Miriam and her book: https://www.miriam-feldman.com/
Growing Up Too Fast: When Your Parent has Serious Mental Illness
Our podcast, Schizophrenia: 3 Moms in the Trenches , continues - and to listeners who asked us, "what about the children raised by parents with SMI?" - we heard you.
This episode (42) is for you!
Guests: Karen Comba, author of The Snipers We Couldn't See: A Memoir of Growing Up with My Mother's Schizophrenia
And Christina Lord, mental health advocate (Canada) daughter of a dad with SZ,
First, your stories.
How has the experience impacted you (Karen writes about life “with footprints on her back”)
How did writing or sharing about it help? Or did it?
How did your experience- and the unpacking of it - inform the work you now do?
What do you most want other children of parents with SZ to know?
What do you want others to know - teachers, practitioners, other adults in a child-of’s life?
How to find happier places for your mind?
Links:
https://christinalord.ca/
https://www.karencomba.com/
Books we mention: (besides our own, Ben Behind His Voices, He Came In With It, and Fix what You Can)
She's Not Herself, by Linda Appleman Shapiro (formerly published as Four Rooms Upstairs)
I'm Not Alone: A Teen's Guide to Living with a Parent Who Has a Mental Illness, by Michelle D. Sherman
Happier Made Simple™: The 7 Core Phrases and Mental Illness in a Loved One
I cry, too - yet there is a way to be happier. The Seven Core Phrases (meant to be said to oneself, not as advice to others, please) and how they help me when our family deals with challenge or disappointment, especially regarding my son’s mental illness.
In the decade since Ben Behind His Voices was published, I've had the opportunity to tell our family story to a lot of people - sometimes more than once, for it is ever-evolving.
If you love someone with schizophrenia, you know this all too well. It is a life lived like a never-ending game of Chutes and Ladders, with moments of rest here and there.
The question I am most often asked, after sharing, is this:
"How do you stay so positive?"
Well.
When Life is Challenging…
It isn't always easy, as you may well know. But - here's the thing that continuously reveals itself to me, no matter what the challenge:
Yes, living happier is a function of what happens to you - no one gets through life unscathed, after all - but it is, eventually, even more a function of what you tell yourself about what happens to you.
And so, I finally wrote a book about it, and it launches officially in a couple of weeks.
In it, I talk about the "Seven Core Phrases" of self-talk that get me through most situations, and keep me hopeful, though realistic - and, yes, happier.
Yes, living happier is a function of what happens to you - but it is, eventually, even more a function of what you tell yourself about what happens to you.
It's how I "stay so positive."
Let me be clear (and I state it up front in the book) - I cry too.
Life isn't about constant happiness. That isn't even a goal. But neither is it about dwelling on the negative when the time for action has passed, nor about stressing about things that may never happen.
So here are the Seven Core Phrases (meant to be said to oneself, not as advice to others, please) and how they help me when our family deals with challenge or disappointment:
These phrases can set your mind down a different path of association and action. In case of severe trauma, you need to process the shock and emotions first.
Be Here Now: I use this when my son is in a good place (enjoy this conversation; savor the moment; enjoy his company) - and when he is not (this is where we are right now - what action do I need to take?)
It Is What It Is: This gets me past the moments of regret (why didn't I see the signs earlier?). disappointment (why was my son robbed of a chance to go to college?), and doubt (why me? why him? why us?). There may be no reason for Ben's illness. It simply is. Now what?
We're All Connected: Other families are going through this too. Other people have the illness. Let's talk about it. Let's help each other. Let's reach out. Let's thank the people who have chosen professions that help us (lawyers, social workers, advocates, psychiatrists, etc.)
This Is Good: Savor the moments when the stars align, and your loved one can communicate, eat dinner with the family, etc. Yes, even during Ben's ten hospitalizations, when the phrase simply meant "enjoy the vacation from caregiving for now." We remember what we savor, and learn from what we regret.
All Will Be Well: Depends on how you define "well." Will Ben ever attain his childhood dreams? Doubtful, at least right now. We learn to adjust our dreams. And I have no idea if the Universe has a "Plan" - but sometimes it helps to believe that it does. Whatever gets you through. As I say in my book: All will be well, just maybe not the way your expected it to be.
Isn't That Interesting?: Curiosity, and even humor, can lurk underneath the trauma and crises. There have been times (especially when in the company of others who get it) where humor has saved me from crashing; when curiosity instead of complaining led me to learn more, do more, find another way.
Whatever Happens, I'll Handle It Somehow: This gets me through more times than I could ever list. Loving someone with schizophrenia means a lot of second-guessing, a lot of waiting to see if the meds work, if they'll come home, if they will be Jekyll or Hyde at the family dinner. So we do what we can to prepare, and hope for the best after that. This phrase gets me through the times where worry is unproductive.
Want the book? You'll find it now on Amazon, in paperback or kindle - but pssst! On launch day Feb 23 the kindle will be only 99 cents for a limited time! - and I am now working on the audiobook.
I hope it helps. Even a little.
Randye
Channeling Grief and Anger into Advocacy and Acceptance
Mimi Feldman, Mindy Greiling and I have been co-hosting our podcast, Schizophrenia: Three Moms in the Trenches, for almost a year now. Our 32nd episode this week has garnered more YouTube viewings in its first two days than any other so far, and guest Jerri Clark, our " Fourth Mom in the Trenches" for this episode, is the reason.
If you want to know more, please subscribe to the podcast on itunes or wherever you get your podcasts, and/or on YouTube. Our facebook page is @schizophrenia3moms.
Here are some of the notes:
What if: the mental health system would pay more attention, take more steps to help , before tragedy, violence, or crime finally calls attention to symptoms of SMI (serious mental illness)?
What if Darrell Brooks (charged with murder after plowing his mother’s car into a parade in Wisconsin) had been helped, and treated, instead of ignored or imprisoned? His mother, Dawn Woods, wrote a letter to the media. She, too, is a “mom in the trenches”. So is journalist/advocate/mindfulness coach Jerri Clark, our guest for this episode.
What if Jerri’s son Calvin had received treatment, despite his “civil right ”to refuse it - although the refusal itself is a symptom of his illness?
She says:
Difficult: Mothering Challenging Adult Children through Conflict and Change, Book Review
Author Judith R. Smith had me at the first glance of the callout quotes:
"You can divorce a difficult spouse. It's much harder to give up on a difficult child."
and
"When a child is diagnosed with serious mental illness, they do not die - but they are changed."
How do we continue mothering, when our children are long past the age when we thought we'd be graduating from the phase of hands-on support? What do we do, what do we feel, what do we fear when our stepping aside could spark poverty, homelessness, even violence for our children?
In this thorough, empathetic account of this important previously-swept-aside issue, Judith R. Smith combines eight years of research and grimly honest stories from mothers of children who have SMI (serious mental illness), addiction, and other issues we never expected to face in our kids.
We learn about the problems presented by not only our own family challenges, but also cultural expectations about motherhood and system failures of support. We feel less alone when hearing the stories and reading the facts. Then, Smith takes us through steps including attitude change, getting support, practicing self-care, and ways to stay safe and possibly even help our grown, difficult, children.
There has never been a book like this. If you're a mother still inside the journey no one wants to speak about, get this book. You'll be glad you did.
Available February 2022, Rowman and Littlefield
Schizophrenia: Nearly Everyone is a “Long-Hauler”
We Need a Cure
The scariest thing about Covid-19, once you’ve been lucky enough to survive it, is a set of residual symptoms that are still being discovered. I’ve heard everything from “it’s a year later and I still can’t taste my food” to “I still get winded six months later and can barely walk up a flight of stairs” to stories of teeth suddenly and mysteriously falling out months after recovery.
People experiencing symptoms like these are called Covid long-haulers. There are Facebook pages and groups where stories and support are available.
But my son, Ben, and others like him? Schizophrenia long-haulers. This is the brain illness that just keeps on “giving” - challenges, changes, symptoms, side effects, loss.
This illness never quits. The residual symptoms sure do beat the active symptoms like psychosis and crisis, but they are still hard to bear.
Everyone is a long-hauler with this brain disease.
We need a cure.
My son is doing okay - actually better than expected - on Haldol now. This older antipsychotic frightens me, because side effects like tardive dyskinesia can be irreversible. Also, it is not known to work on the “negative” symptoms of schizophrenia (things the illness takes away from the person, like ability to feel joy). Still -it’s not too bad.
Some good news: (must mention, Ben no longer lives with us, so some of this may be due to the excellent staff at his group home, and a life less dependent upon our family role as landlords etc)
I can converse with him. Actual give-and-take conversation.
We have actually watched an entire movie together.
He eats my cooking again, after years of saying “smells great, I’ll have some tomorrow” (I think he had some sort of belief about my food that prevented him from ever taking a bite in those years).
He has also gone swimming again, and plays beautifully with his nieces and nephews. In fact, they have a relationship with “Uncle Ben” for the first time in years.
Haldol is available as an LAI (long-acting injectable) , so Ben isn’t faced with a daily decision as to whether he “needs” antipsychotic meds or not.
But, some of the sadder news:
I do see some trembling in his hands now. Would he ever be able to work as a waiter again, the job that kept him afloat before Covid closed restaurants?
He is suspicious of doctors, dentists and any medical testing. This is fairly new. He will not have his teeth cleaned.
When he isn’t hyper- focused on something I see the eyes darting around the room again, and wonder what he hears and/or sees. He will NOT talk about this, or admit to it.
He talks once again about unrealistic plans - like opening his own restaurant, becoming a college professor.
This illness never quits. The residual symptoms sure do beat the active symptoms like psychosis and crisis, but they are still hard to bear.
Everyone is a long-hauler with this brain disease.
We need a cure.
Daring to Hope Again: Faith or Foolishness?
The game of Schizophrenia Recovery Chutes and Ladders (or Snakes and Ladders, for you Brits) continues.
In the past few weeks, Ben has climbed some ladders, made some progress. Yesterday's family visit was full of simple pleasures again:
a car ride that was full of conversation, not the torture of awkward silence and small talk
Ben and a friends watched a movie in our living room and actually made it through the whole thing
We talked about his future, his feelings, his sobriety journey (now counting again, 15 days)
Ben was less defensive, more forthcoming
I brought up my concerns about his current med (Haldol) and my wish that someday he might try Clozaril again so as to avoid the side effects (tardive dyskinesia, mainly) of the Haldol - and Ben seemed to listen. (not agree, but he did listen)
These days are miracles. These days give me hope, though I've learned not to predict beyond a good day.I don't predict. But I can hope.
I can hope that Ben will continue to value his sobriety and the meetings that help him.
I can hope that the side effects of the Haldol are not permanent.
I can hope that he can again be a part of family celebrations.
I can hope that, perhaps, one day, he will gain insight into his illness and serve as an inspiration to others.
I can hope that he will, again, be able to work, to have friends, to feel purpose and joy.
I can hope for a cure for schizophrenia.
Hope is not foolishness. Hope is a celebration.
If I'm wrong, at least I'll have had a day of seeing my son's smile again, or actually enjoying talking with him, of seeing that he might be able to get some of his life back.
And that I can't do it for him. All I can do is love him (always), set limits (whenever I have to), and do the behind-the-scenes advocacy that is necessary to keep him afloat.
(where are his social security benefits? Does he have money to pay his rent? Can he work again someday? Where? How? Are there activities he can participate in right now, to give him the structure and purpose he lost when he lost his job due to Covid and then turned to smoking weed instead? ....the list goes on. We orchestrate behind the scenes.)
A good day. I'll take it.
"Mom, My Future Seems So Bleak": Feeling the Heartbreak
My son. He is trying to hard to get his life back. If he weren't trying so hard, maybe then I could detach - let go just a little bit more than I've already trained myself to do.
But it's heartbreaking. For me, sure - but mostly for him.
The trouble with regaining some sanity (or sobriety, for addicts) is that your vision, when examining your life, clears. That, unfortunately, can hurt like hell.
I can feel why, sometimes, it may feel easier to just fall down the rabbit hole of non-treatment and go back to a problem that's more familiar: getting out of the hospital.
Square One (or two, or three), when you've climbed so far ahead of it in the past, is really a hard spot to land back on. Ouch.
The trouble with regaining some sanity (or sobriety, for addicts) is that your vision, when examining your life, clears. That, unfortunately, can hurt like hell.
That's part of why a fresh obstacle to Ben's renewed recovery journey (after the Covid-19 fall) is now: getting clean. He has returned to smoking pot - never a good sign - which brings all the usual "side effects": lies, denial, the illusion of accomplishment, poor decisions, loss of money, lack of motivation.
Shit.
Road to recovery…Far from Clear
The first signs were during a home visit - halfway through a fantastic visit, after Ben "took a walk to Starbucks", he returned home completely stoned. And denying it. I took him back home and told him he could lose his placement in the group home, and also I would not be allowing him to visit until the truth - and a plan of action - came through.
One day later, a very contrite Ben called to apologize, in tears, and ready to tell the truth and "get clean"...and he did - for 35 whole days. He even went to meetings, and shared for the first time ever. Yeah, maybe "it's only pot", but for Ben it spells disaster.
Then...a relapse. He took 2 hits from "some girl on the street corner" (after refusing once, but then he caved) because "I thought it wouldn't really make me seem stoned, and it might make me feel better about my life."
Another call from his Group Home.
Another frantic message of denial from Ben
He can lose his housing. He lost his home visit. I feel stuck in a cycle of Groundhog Day-like repetition.
I gave Ben a day to come clean with the truth - and he did. We talked for over an hour. He is so angry with himself. He regrets giving in to temptation. He says all the right things...but he has said them before.
Still - what breaks me apart are two things: his voice, cracking with tears and emotion (rare for those suffering with schizophrenia), and his statement:"
Mom, My future just feels so bleak."
Oh. My.
He has lost everything he works for years to build - his work, his car, his friends, his sanity, his place in our home -- and months of his life. Unemployment is a huge blow - I've been there, and so has my husband, and maybe so have you - but imagine going through it when you've also "woken up" from the longest hospital stay of your life, to find that your world has fallen apart.
And now - some steps we've all agreed to, to provide more purpose and structure. Yes, he wants to work again someday - that waiter job was everything to him (but can he work? with hands trembling from Haldol? we shall see) - but for now, all I can do is remind him that:
he has rebuilt his life before, and can do it again
there are people who want to help
Getting too cocky, and thinking you can get sober alone, seldom works for him - and is often a sign of danger.
We love him
For now, it is good to sign up for some activities offered to him, even if they fall short of the full-time work he used to have.
Here's where we are. Ben is in a group home. He is rebuilding again after a 5 1/2 month hospitalization.
The Four Pillars, our present day version in this new Recovery Journey:
Treatment: Haldol by injection (different medication for Ben than the one he'd done so well on - in my eyes - before, but he swears he "likes it better".
Plus Side: Injection form much easier to manage (time-release)
Minus side: I am seeing tremors (could become permanent). Ben hides these, and denies their existence.
Structure: Some. Group Home meetings, and now some "Anonymous" meetings. He needs much more structure. Don't we all. He fills his time taking long walks, but his life is too aimless (considering pre-Covid he worked full-time)
Purpose: He was stripped of it when Covid cost him his job. Purposelessness sucks.
Community/Love: Well, he still has us, his family. But now it's weekend visits, and only if he is clean and sober. He has lost the right to visit us more than once - along with my trust.
So - we move ahead. With new steps. One day at a time.
2 days clean/sober, and he has also learned some things. Hopefully they will stick.
Hope for "Normal" Days Springs Eternal
"Mom, I sometimes I thought I'd never actually have a pleasant day with Ben again. Today was so great!"
Exactly my sentiments, honey.
Families of those with Schizophrenia know: "normal" days are miraculous. And we treasure. Every. Single. One. Because, well, we might not get more of the same. no guarantees.
Hope springs…and sustains
Blog followers here know that we've had quite a few, um, adjustments to make re Ben in 2020-21. From full-time employment to hospitalization, to back in group home care...and now, addiction to contend with. It has been a tough year for us, sure --- but so much worse for Ben, especially now that he is "well" enough to realize that his life has gotten so messed up.
He has lost so much.
Stupid Schizophrenia. Thief of lives. Robber of relationship. Obstacle to useful employment. And so much more.
And yet. There is hope - and moments to treasure again. Grateful, grateful for:
Ben, 25 days clean now. (his addiction is marijuana). One day at a time. He is going to meetings. Fingers crossed. But - wow - it is so different when he isn't stoned.
Two days in a row of family fun - yes, fun! Ben is on Haldol now - not my favorite, as I fear the permanent side effects, but Ben seems happier on it. Letting go of control...as best I can. It's his life. But I must say that things are better than expected, even though Haldol doesn't do much for the "negative symptoms" of his brain illness.
But - some miracles in the past few days, on family visits:
He went swimming! He used to love it so much as a boy, but for some reason hasn't gone in the pool for five years (I suspect some sort of psychosis belief that kept him away, but I'll never know for sure) -it was always, "Maybe next tiem" - but he went swimming with his young nieces and nephew, and actually played with them. Played!
We did a family trip to the local Aquarium and Ben was actually helpful - the kids adore him, and he was present and involved. And - during lunch, he turned to his sister (as the kids were doing their "I-haven't-been-to-a-restaurant-since-Covid- and-forgot-how to-behave" routine) and said, "wow, sis, you have your hands full, don't you?"
Empathy!
If you have a relative with SZ, you know what a miracle this is.
Yeah, he's trembling a bit, and I fear the presence of tardive dyskinesia - a possibly permanent side effect of the med Ben is on.
But all we have is today, and what is, is.
So I'll take the miracle of having made some more good memories with my son. Grateful And always hopeful, and ever watchful.
Guest Blogger: CJ Hanson, Mental Health/Brain Illness Advocate
One day into June, and the official #MentalHealthAwarenessMonth is over - but the fight is far from over.
Please welcome guest blogger, C.J. Hanson, with these thoughts regarding her brother who has serious brain disease. CJ is one of the authors in Dede Ranahan's award-winning book,
"I have strong opinions regarding the many different causes for the continual denial of help and easier access to real treatment for my brother since the beginning of his trauma and brain illness of Schizophrenia and Anosognosia.
We initially thought the care he needed was going to be available to him given how severe his multiple disabilities including having lost his eyes in an accident and then brain illness.
We each have our own obstacles. But, like most families - access to that elusive help - was slammed shut on us because Mark is an adult who happens to have anosognosia related to the brain illness.
Waiting for him to figure out what is best for him.. what is safe for him... that he even has a serious mental/brain illness... will never happen.
CJ Hanson, Mental Health/Brain Illness Advocate
No one can understand the respective roles that we are each left to play amidst the absolute expectation from society that we should just innately have all the answers, when we have a loved one with SMI/SBD - an expectation that we are fully capable to physically house and care for someone so floridly psychotic after he has fallen 34 years into the abyss and the tiniest of cracks of his mental illness. Our shattered and fragmented Mental Health Policy & Laws which includes abandoning the most vulnerable of those among us and their families is cruel.
Many of us are just family members struggling to be what we are not. - Medical professionals, Neuro Psychiatric professionals, Medical intervention, Legal and Financial advisor, Psychiatric Technician, Social Worker, Protector, Nurse, even Guard - day and night. Every day and night.
From what I have seen some of the top advocates for Mental Healthcare Reform are those who have paid the ultimate price already... either the loss of their loved one to suicide, abuse, injustice or just completely and forever lost in their illness.
Some family members, advocates and activists are still smack in the middle of their struggle to avoid those outcomes.
But, we are all advocates and activists - for Serious Mental/Brain Illnesses and the change towards quality of life, comfort, justice and fairness in #MentalHealthcareReform. Which means including the family members."
~ CJ Hanson
PS - I hope that my friends, group members, and followers will visit the new Facebook page which will follow the development of the movie documentary and give us a "like," follow it... and if you are moved - to contribute to the production and success of the documentary. Please share the link to the page on your timelines and to your friends too for the success of this important project. We will be successful with your help!
https://www.facebook.com/noonecaresaboutcrazypeople
#NationalShatteringSilenceCoalition
Oprah, Harry, and Schizophrenia: The “Me” My Son Still Can’t See
The Me You Can’t See
Have you seen the new docuseries on AppleTV+, “The Me You Can’t See”
First of all, thank you, Oprah and Prince Harry, for joining the ranks of advocates who are becoming more open, honest, transparent about mental health issues, barriers, and some solutions. In this 5-part series, people from celebs (like Lady Gaga to the Prince himself) to “regular folk” talk about trauma, challenges, heartbreak, and where they are now.
This is brave. This is eye-opening. This will help some folks, diagnosed with mental health issues (or those who know, treat, or love them) to understand and know they aren’t alone.
Thank you.
And yet.
Does it go far enough?
I am hoping for a second series, where more illnesses are explored, uncovered. Especially schizophrenia in those who have yet to be aware that they have the illness.
As we’ve covered often in our podcast, Schizophrenia: Three Moms in the Trenches, and in the books and blogs we share, one of the hardest things about schizophrenia is that the first step often can’t be taken: the step of awareness. Anosognosia is the condition that keeps Ben, and countless others like him, shielded from that awareness - and from accepting treatment unless somehow coerced into it (even by love).
Oprah and Harry - next time - and I do hope there will be a next time - please talk to the families of those affected by severe mental illness.
This is the episode I’m waiting to see: the person diagnosed with schizophrenia who has yet to be aware of it. Along with the family members who still love them and feel powerless to help.
We cry, we fiercely guard, we coerce, we lose sleep, we go broke.
We live through grief, live sometimes in fear, we lose our own futures, and we bounce back a zillion times - all in the name of love, and in the hope that more people - researchers, practitioners, lawmakers, first responders - will learn from our heartbreak and advocacy, and continue to prioritize (and fund) services and science that will help our loved ones, and our families.
Ben (my son), as you may know from following this blog, recently was released from a nearly-six-month psychiatric hospital stay (almost unheard of in this country) and has slipped from a relatively normal life of work and semi-independence to one of a group home bed and starting from scratch.
Still, he does not believe that going off his meds had anything to do with the breakdown he experienced in August. He refuses to go back on the meds that he was treated with when he managed to have a clearer semblance of a life. The light is no longer there in his eyes, but he doesn’t feel the difference.
While he has said he “struggles with symptoms”, he won’t say what those symptoms are. He becomes paranoid and cagey if I ever bring it up. I’ve learned not to.
I’ve learned to appreciate whatever crumbs of my child I can get, and am grateful every day that he is in a place (for now) with a staff trained to help him - even if he refuses much of that help.
According to NAMI,
When we talk about anosognosia in mental illness, we mean that someone is unaware of their own mental health condition or that they can’t perceive their condition accurately. Anosognosia is a common symptom of certain mental illnesses, perhaps the most difficult to understand for those who have never experienced it.
This is what makes schizophrenia so difficult to treat - the “rights” of patients to refuse the treatment that would help them the most.
If we applied these “rights” to our parents or other loved ones with dementia or Alzheimer's, they’d be living in an unsafe world. So we don’t allow that to happen.
Well, untreated, so is Ben. And so are the families of people diagnosed with SMI (serious mental illness).
When you cover schizophrenia by interviewing someone who is in treatment, and aware of their own illness, you don’t tell the whole story.
This is the episode I’m waiting to see: the person diagnosed with schizophrenia who has yet to be aware of it. Along with the family members who still love them and feel powerless to help.
Thanks, though (really, I mean this sincerely), for the brave steps you have taken so far.
Let’s keep going.
The Extra Innings Movie - and Podcast
A few years ago, I had the honor of speaking at an event to increase mental illness and suicide awareness, and to built support for an independent film called "Extra Innings." -described this way on imdb: "Set against the enchanting backdrop of 1960's Brooklyn, Extra Innings tell the story of a young man who is caught between pursuing his dream (baseball) and staying devoted to his Syrian Jewish family that is afflicted with mental illness."
I have stayed in touch with the creator of the film, and last night was honored to be a guest on his podcast. We talked about schizophrenia, family, stigma, support, and so much more.
Listen to the Full Episode: talkradio.nyc/shows/extra-innings
You can see or hear the podcast here:
or here.
Meanwhile, about the movie:
It did get produced and released - and was winning awards all over the place and set to go to movie theatres...and then Covid hit. We all know all about that. But - the good news is that you can now see it on Amazon Prime. Don't miss it!
As for the podcast, here's what Albert had to say:
“The love is pure, but the rest is difficult. I wrote it for families to not feel so alone.” Randye Kaye on what motivated her to write her book chronicling the journey of the development of her son’s mental illness.
Check out this exclusive clip of Extra Innings: Covering All the Bases! This week’s guest was actress and author, Randye Kaye.
Randye Kaye makes her living as an actress. In 2011, she published her memoir Ben Behind His Voices: One Family’s Journey from the Chaos of Schizophrenia to Hope, based on her own experience understanding and living with her oldest child’s schizophrenia. She hosts two podcasts: The Life Talk Show and Schizphrenia: Three Moms in the Trenches.
Find More about Randye Kaye
Website: randyekaye.com
Albert Dabah is a certified life coach and therapist who began his career as a social worker. He founded his video production company, Simba Productions, in 1979, and recently directed and wrote his first feature film, Extra Innings, which is based on his own life.
Life Coaching: adabahcoaching.com
#ExtraInningsMovie is available to stream on Amazon Prime, and on demand at Google Play, Fandango, Apple TV, Vudu, and DVD through our website at extrainningsmovie.com
Watch the trailer! bgpics.com/movies/extra-innings/
Watch Extra Innings: bgpics.com/movies/extra-innings/
Out of the Hospital, Not Out of the Woods
It has been almost four weeks since I picked Ben up, curbside delivery (not allowed to enter the unit due to Covid) from his over-five-month stay in a “behavioral health center” (AKA psychiatric hospital). He was so full of hope, the day so full of promise - but we family members know to enjoy the moment, and prepare for a fall.
Man, I hate to be right about this. But I knew - I knew - he was on the wrong medication, and it was only a matter of time.
Timetable of deterioration:
(first few days covered in more detail in the earlier post):
It doesn’t take long to lose ground
Thursday, Feb 4th - pickup, home to pack, delivery to new housing I’ll call B Home (very very grateful for that arrangement, don’t get me wrong). Ben seems excited and open to his new life.
Friday, Feb 5th - I drop off a few items he forgot, and already Ben seems off. He’s on a time-release injection of Haldol, and wasn’t kept in hospital long enough to observe how to time the next needed dose.I call to inform the psychiatrist via Ben’s case manager (who can ever get the actual doctor on the phone?) and am told he’ll get back to us on Monday. That’s three more days that Ben can deteriorate.
Monday, Feb. 8th - the doctor has done nothing. No oral boosters prescribed, no change in the next injection date. Ben seems not much worse, which is good, I guess - but he is still not good. Families know.
Thursday Feb 11th - I drop off a few shirts to Ben at B Home. He holds it together enough to talk to me through the car window.
Good news: he is wearing a mask.
Bad news: he has gone on a shopping spree for hoodies. He has about 60 hoodies already, folded neatly (by me, while he was hospitalized) on a shelf in his old room.
Man, I hate to be right about this. But I knew - I knew - he was on the wrong medication, and it was only a matter of time.
He is stable (ish), but it’s like the nine years he spent getting off Disability and working up to full-time employment have been erased completely, like an extended version of the plot of Groundhog Day.
We still have not heard a peep from his psychiatrist.
Feb 15-19 - I am so grateful that Ben is in B Home, and not with us. I think my heart would break every day seeing him like this. Texting and phone class, even facetime, are helpful. He’s pretty good on the phone.
I do have a long conversation with the B Home Social Worker, who seems caring and informed. She actually listens to me as I share Ben’s medical and work history. She is amazed that he used to work full time. I’m sure she can’t see that possibility in him, the way he is now.
Meanwhile, the money questions pile up. Did Ben have Social Security reinstated? I’ve been working on this since October.
I speak to Social Security, to DSS, to his benefits manager, to the residence staff….and everywhere there is a different story.
Ben lost medical coverage...no, wait, maybe he has it.
Who will pay his rent?
Are his medications covered? Yes, they are. No, wait, they aren't.
One system says yes, the other hasn’t gotten the memo.
This is a SNAFU paperwork nightmare.
I am told that if Ben weren’t on the “fast track” these decisions would take two years. Two years!
Feb.20-24.
A new wrinkle.
Ben’s case management team is suddenly being disbanded. He has been within them for 18 years.
Now, a whole new team to train. I hope they’ll hear our story. I hope they are better.
I hope the doctor is more attentive, knowledgeable, helpful, caring.
I am wishing for a lot. As ever.
Meanwhile, Ben’s “rent” has not been paid because no one knows where his benefits stand. I write out a check for almost $1200 and mail it in to B Home. I cannot afford this. But of course I pay the bill.
And, Ben is failing. The B Home staff tells me he is twitching, gesturing with his hands, mumbling, eyes darting off to the side. Also, He’s isolating in his room whenever he can, listening to his music.
This, my son who waited on a full station of tables just a year ago and kept it all straight and came home full of joy about the social interactions.
I know these signs. The voices are getting louder.
God, please help my boy.
The psychiatrist has yet to order oral Haldol boosters or move up the injection.
This didn't have to happen! Yes, sorry but it's true, I told you so!!!!
Feb 25 - finally, Ben is scheduled to get his next long-acting Haldol injection. It’s happening tonight.
But no.
At 7 pm I get a call from B Home. The pharmacist doesn’t see any medical coverage and won’t fill the prescription. This just becomes a thing at 7 PM?
“Don’t worry,” they say. "If he gets more symptomatic we’ll just get him back to the hospital."
What?
But no one even knows if he has medical coverage. The case is still being “decided”, according to the DSS case manager I spoke to yesterday. This has been going on (I repeat, sorry) since October.
And this didn't have to happen! Yes, sorry but it's true, I told you so!!!!
Many many phone calls later (bright spot: the benefits manager calls me back even tho it’s past her workday hours), I am assured this will be straightened out by morning. If Ben gets through the night without full-blown psychosis.
If.
I hold my breath. But I do sleep. The benefits manager told me to.
Feb. 26 (today)
We think he’ll get the injection today. We think it has been straightened out, that the pharmacist will fill the prescription, that the nurse will arrive, that Ben will not run away from her (that has happened before)..
I’ll believe it when I get the final word.
No, out of the hospital does not equal out of the woods.
And so many others have it so much worse. At least Ben has a roof over his head, staff to manage his care, a family that loves him.
But it could be so much better.
Quoting Willy Loman (again, and just as fruitlessly it seems) from Death of a Salesman:
Attention must be paid.
The Public Cry: #freebritney! Is There More to the Conservator Story?
We become conservators to rescue.
Listen, I want Britney Spears to be happy too. She's incredibly talented, seems nice, obviously loves her children, and has worked her ass off pretty much all of her life. And, yeah, her dad seems like a controlling asshole. Also, it has to suck to have your adolescence questioned and paraded all over the media. She was not treated with respect, to say the least. The paparazzi and press were shameless in their interference - and, well, sheer gall. Anyone might crack under that kind of pressure and scrutiny.
(Imagine if all Your teenage love starts and fits has been plastered over the tabloids. I mean, Seriously.)
But, after watching Framing Britney Spears (and to channel Carrie Bradshaw), “I couldn’t help but wonder.....” even now, are we getting the whole picture of her conservatorship?
This is not a popular take right now. And I’m not saying that Brit shouldn’t be “set free”. Honestly, it’s none of my business.But, since I am a conservator myself, I’m just saying there might be more to the story. Have we fully seen in that documentary what a conservator can do to help? To avoid disaster? To protect the conservatee? We have not.
Even Brit herself, speaking out after the documentary aired, has said “everybody has their story.”
Here’s mine.
I applied for conservatorship in 2003 when my son Ben was about to sign papers to “set himself free” from the psychiatric unit in the hospital. He was psychotic, confused, a danger to himself - but would have been released anyway because he had “rights.”
But by applying for conservatorship and right to treatment, I bought him some time - time to stabilize and to plan for discharge.
I became Ben’s conservator (of estate and person) and fought for his “right” to be treated for a serious brain illness - and kept fighting. Because of that, he finally was stabilized enough (5 hospital stays later) to be placed in housing where he could begin to rebuild his life.
And, I had the right to information each time he was hospitalized again. Without those papers, I’d not even have been able to know where he was.
In the 18 years since that decision (one I have to renew every year), I’ve stayed as far as I can from making decisions for Ben. Not all conservators decide what a person eats for breakfast (like Britney's father in the documentary). However, I have been able to step in and help when necessary.
Some examples:
Ben thought he was “helping a co-worker” by co-signing a car lease agreement for her - without my knowledge. When she defaulted and he was hounded by debt collectors, I was able to get him out of the agreement.
Ben decided to sell a perfectly good used car we had gotten for him (he paid us back, bit by bit, and had been free and clear) and lease a brand new one....to the tune of almost $800 a month.He went over the mileage and “solved “ that by leasing a more expensive one. We have to declare bankruptcy to get him out of that debt.
He is a shopaholic. I know it makes him happy to feel normal...but did he really need a set of pool balls and cues when we don’t even have a pool table? I can’t really stop him, but I can keep enough money set aside (if he has any) to make sure bills are paid.
He has now been hospitalized 9 times. That’s a small number compared to others I’ve seen. But my conservatorship gives me the right to know medical information, from the smallest detail (yes, he is a patient there) to the larger issues of what a discharge plan is.
I can take charge of getting his disability payments back. This is absolutely essential right now, as he is back to square one and has no other income at all.
While he was in the hospital, I was able to keep up his credit card payments ((of course, he was maxed out and only paying minimums)
“But (I hear you saying in your head) why don’t you let him just make mistakes when he hits bottom won’t he learn his lesson? The answer is… No. With schizophrenia, even treated schizophrenia, learning from your mistakes is often not part of the picture. I wish it were.
I do not decide what he eats for breakfast, who he hangs out with, where he goes. I am a safety net, and he has fallen many times. Mostly I let him make his own decisions, but within reason.
Like today:
“Mom, did I get a stimulus check? Where is it?”
“Yes, and I put it aside to pay your rent until your social security is approved.”
“Oh, ok.”
(Because I know, from experience, that if that check is at his disposal he will not rest until it has all been spent on clothing he does not need. trust me , I know. I cleaned his room while he was in the hospital. He could also use it to buy pot. Nope. Not on my watch).
Conservators are not all dictators or assholes. Most of the time, we don’t even want the job. But someone has to do it, and if we can prevent total disaster we step up to the plate. Most of us strike that balance of letting go and stepping in. or at least we try.
So - i feel for Britney, I really do. But that documentary was very one-sided. I would just need to hear the other side of the story. Wouldn’tyou?
He's Out! But For How Long? Family Input Ignored.
It was so much easier then…
“Dear Mom, and whoever else may or may not be listening. This goes out to my mom with deep heart-feltedness. For whatever I’ve done in the past, I’m extremely and genuinely sorry for, and will forever be.”
I have this recorded on my iPhone.
Why? Because one of the first things Ben did after I picked him up from West Hills Behavioral Hospital a few days ago was to apologize.
I was so shocked I asked him if he’d say that again, into the phone, and make it official. He laughed (laughed!), and said sure.
It was a good moment. I’ve learned to treasure those, since they tend to be fleeting.
I was right. Unfortunately. Shit.
Ben had been in the hospital for over five months this time. It was a nice vacation for us (sounds cruel, but if you e been there you get it), though beneath it all is my mother's heart that hurts for my son and all he'd lost after losing his full-time restaurant job to the Covid economy. I’d watched the downward slide for months, as he bravely (in my estimation) held on to hope and tried to fill his days with purpose. That’s didn’t go so well. Marijuana use increased, and so did his determination to not take his meds. All kinds of tricks, and we were powerless to do much except supervise, nag, accuse, try to outmaneuver him. It had worked...for awhile.
Now, after the hearings giving us right to treat and commit “over objection”, Ben finally stabilized - but not on the medication that had brought him back to a place where he could work as a restaurant server....and fool people into not knowing he has this devastating brain illness: schizophrenia.
No. Because he “doesn’t like the side effects “ of that medication (and I don’t blame him, but still...), he has chosen (and had the right to) an old antipsychotic, Haldol, which works okay but can have even worse (and permanent) side effects.
Yes, even in the hospital, we can win the right to treat, but not to choose the right medication. He has “rights” , which cause him harm.
This medication has brought Ben back, sort of - and it breaks my heart to see how hard he's trying to seem like his old self - but he definitely is not the same. As my daughter says, “I look in his eyes and he just isn't there.”
Best - and hardest - decision we made was to have him discharged to a group residence (let’s call it E house)instead of to our home where he'd been living for the last nine years. He is doing his best to be enthusiastic about this. He has not once guilted me, not once complained about his new situation. Yet. I’m crediting the group work he did in the hospital, for that (and for the apology).
Still, it’s such an echo of where we were back in 2003, when Ben was accepted into his first residence. The house seems nice, the staff seems caring. Hard to tell some of the staff from the patients...until you look and listen a bit more closely. Ben has his own room (for now), and I’m grateful there is a plan in place to ease him gradually into independence.
But. And there is always a but.
He is slipping. He’s on a time-released injection of the haldol. This is good, until it starts to wear off. And he wasn’t kept in the hospital long enough to gauge the half-life of the injection. Daily boosters can be given orally, but he hasn’t been prescribed any daily medication except something to prevent side effects (like twitching.)
And every day since I dropped Ben off, he gets worse and worse. And it has only been 4 days.
I’m spared long visits because of the pandemic, (sorry, but it’s true. Visiting is painful when he deteriorates), but when I dropped off his Medicare card the day after he was admitted I could see it. Couldn’t focus, trying too hard to be sociable, repeating things. I know the signs, believe me. And...I’ve seen him when he’s truly functional (or what passes for it when your brain is filled with constant interference) and believe me I know the signs.
We cannot wait for his next injection appointment. It will be too late. We need to fix his treatment NOW.
I call the staff, from their parking lot, to tell them what I see. Even though they barely know him, and have never seen him well enough to handle a restaurant rush and still get kudos on Yelp, they see the decline too. They agree with me. So....I call his case manager.
This is a a Friday.
I’m told the psychiatrist (Dr. K) will check on him on Monday.
I say Monday will be too late.
Case manager says he'll talk to Dr. K and get back to me.
Of course he doesn't get back to me.
The staff at E house tells me not to worry, as they will "get him to the hospital if it gets too bad."
This is exactly what I am trying to prevent.
It’s like I have to train a whole new set of staff.
Hello, please meet my real son. This is the one who, when balanced, can get a 50% tip from a happy family. Who can make a great speech at his sister's wedding. Who can muster some genuine caring and empathy for others.
When treatment works, he is more than just “stable”. He is wonderful.
And right now he is neither. He needs better medication and he needs it now.
It’s such an echo of 28 years ago when he was first placed in a residence after his 5 hospitalizations in that one year.
Only then, he was 21 and I was 51. Now we are approaching 38 and 68. In all that time, are there no other options? Have they not realized that family input matters?
When will this horrible illness get the attention it deserves?
Five Months a Patient (Psychiatric Unit): Daring to Hope Again
One week from today, Ben will be discharged from the longest hospital stay of his life. Five months. Five months! Believe me, I am grateful. Grateful that he was safe, cared for, and somehow has returned from the abyss of his illness. Again.
Not gonna lie, though: we’re also very grateful for having had a break from living with him. What a blessed empty nest. No staying up til 3 AM to make sure he takes his meds. (Up until Covid hit, Ben had worked as a restaurant server, thanks to those meds he hated). No cigarettes on the front porch. No huge messy vegetarian cooking marathons. And, mostly, no tension in the house from secrets kept, delusions hidden, resentments festering.
How, after nine years of success, did Ben wind up at square one, delusional and certifiable? I can blame Covid-19 (see this earlier post) for the job loss, the structure crumbles, the community scattered, his purpose stolen – but, truthfully, he was teetering on the brink of the rabbit hole even before that. Excessive pot use, self-caused financial stress (he leased a Lexus? Really?), and mostly – mostly – resenting and cheeking the medications that provided the foundation for his ability to function in reality. Every night my husband or I could feel the hatred coming from Ben as we supervised his medication he desperately wanted to not need, all his charm having been used up at work and none left for his family.
But there’s only so much you can do if he backwashes into the water and then swears he didn’t.
We got by. We all squeaked by. Until August 29, 2020. Another night spent in the police station, calling the on-call psychiatrist, watching my son disappear before my eyes. Again. Talk about the worst Déjà Vu ever.
Fast forward, I guess…past more court hearings, renewed conservatorship, Ben’s refusal to go back on the meds that work best for him, awkward zoom calls (no visiting allowed, thanks Covid), paperwork trails to get him back on disability and out of debt. Where are we now?
He finally seems stable again – but he’s on Haldol, a medication that can have devastating – and permanent – side effects. Also, it doesn’t help much with the negative symptom of schizophrenia, so I’m not a fan. But Ben has refused to do the blood draws required to be on Clozaril. So here we are. And - so far, so good.
It seems okay. He called me yesterday – three times, as he needed a favor – and we actually had a conversation: about his bank account (yes, I deposited money so he won’t be overdrawn), his car (repossessed, and he’ll have to declare bankruptcy and start over again), his housing (back to a group home, which has thankfully accepted him), about origami (he taught everyone on the unit how to do his favorite creations, something he recalls from years ago), and even about politics. He is aware that we have a new President, and that in itself is a miracle, since five months ago all we got out him was the occasional grunt and suspicious staring and mumbling to his voices.
When Ben learned that I had taken care of his affairs, he said, “Mom, you’re the queen of the world” – and he meant it to be funny, not a delusion. I have my son back – well partially. As always, I'll take it. Better than nothing.
In one week, he gets placed in a residence with a day program included. He has no car, no job, and will be living a half-hour from us. But it’s better for him, and for us. I hope and pray that he doesn’t walk out the door of that place when the nurse is coming with his medication. It had happened before. And then– back to the psych unit. The revolving door.
I have my son back – well partially. As always, I'll take it. Better than nothing.
But, for now – we hope. And express thanks to the staff that has kept him safe for five months, the medication that seems to be working, and that there was bed available for him.
Can things fall apart again? Oh, heck yes, you bet they can. But dare we hope?
Absolutely. We dare to hope. No use predicting disaster (then we’d have to go through the emotions twice, and all we’d get is the booby prize of having been “right”. (Ugh) – all we can do is our best to prevent it.
Welcome back, Ben. I’ve missed you. Not the illness – I hate schizophrenia with all of my being. But now that I see glimmers of my son again. Yes. I’ve missed that.
One step at a time. And avoid the rabbit holes.
Breakdown: The Right Title for a Much-Needed Book
I've often wondered what treating patients with SMI (Serious Mental Illness) is like for medical professionals. I want to know, too, what the intake process is like for clinicians, and whether they feel as frustrated with the system as we family members do. This book answers these questions, and more.
Through it all, author Lynn Nanos, L.I.C.S.W., shows such concern, knowledge, and caring for people like my son Ben (who is diagnosed with paranoid schizophrenia), that I kept wishing she were on the team treating and caring for Ben right now.
I had to sharpen my pencil several times, I underlined so many facts and observations.
Five Shocking Facts
Five things that either stuck with me or surprised me - and, after nine hospitalizations for my son Ben, I thought I knew it all...
Often the "easier-to-manage" psychiatric patients get admitted, instead of those who need the help the most, because they are cheaper and less difficult to manage. Those admitted include "malingerers" who just want to get off the street for "three hots and a cot" and can fake psychosis.
Connecticut (where I live) is one of only three states in the U.S. (along with Maryland and Massachusetts) that do not have laws allowing AOT (Assisted Outpatient Treatment), something that most definitely would benefit my son.
Yes, untreated schizophrenia can increase the incidence of violence. And often, when the voices tell a schizophrenia patient to harm someone, it's someone they know...and usually love.
Regarding RLC's (Recovery Learning Communities, often staffed by "peer specialists who endorse the possibility that signs of psychosis are normal"): " Researchers found no significant benefits...to help the seriously mentally ill population"- of which my son is one. I live in fear of those who would try to "teach" him to get off his meds. And yet the government allows antipsychiatry to infiltrate programs it runs. (Chapter 18)
Why do psychotic people not engage in treatment? Nanos lists 17 reasons, and "stigma" was not among them. She argues (backed up by research) that stigma is overrated as a reason to not seek treatment for the seriously mentally ill. She says not one patient has ever mentioned that as a barrier to seeking help.
Lynn Nanos knows her stuff, truly cares about her cases, and fights for what's right - while fearless in exposing the cracks in the system.Highly recommended reading.
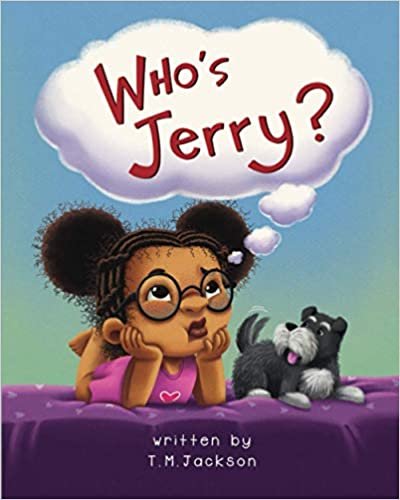
Who's Jerry? Helping a Child Understand Mental Illness
Mommy is acting funny.
Daddy yelled at me for no reason.
Why is Mommy in the hospital?
How can a brain be “sick”?
Finally, a picture book for children that addresses the most secret of secrets: my parent has a mental illness.
We follow little Imani through her confusion, sadness, loss, and adjustment as her mother reacts to her inner voices (one named Jerry), lashes out at her daughter, goes to the hospital for treatment, and finally returns home, with her illness under control. Through it all, Imani’s father provides support for her.
if you know a young child who is dealing with this in his or her family, this lovely book is a great place to start. It could be the key to opening the conversation we seldom know how to explain.
"Fix What you Can": Apt Philosophy for Family Mental Health (and book review)
I highly recommend this memoir for anyone who wants to know more not only about the family experience with schizophrenia, but also why it can be such a long and difficult process to change the legal barriers to getting our loved ones the help they so desperately need (but think they don't).
Mindy Greiling and I have many things in common, though we've never met. The biggest shared experience: we both have sons with schizophrenia, and we haven't given up on them. As she says in the epilogue of her new book, we are "the best mothers we can be."
As any parent knows, good parenting is a shifting balance between stepping in and letting go. When mental illness and substance abuse enter the picture, that balance is ever more precarious. And "happy endings" are, often, only fleeting respites from trauma, until the next chapter begins.
Still, we love.
Still, we hope.
Still, we fight.
Mindy, for much of this memoir, is able to channel much of this fight into her work as Minnesota State Representative - a position she held for twenty years, advocating tirelessly for improvements to the mental health laws in that state. She's received more than eighty awards for her legislative and advocacy work. She has so much good reason to be proud.
But her son, Jim, still has schizophrenia. That, as we know all too well, sucks. And in this memoir she is raw, real, and informative about her family's journey, and also her work to enact changes in the system.
I highly recommend this memoir for anyone who wants to know more not only about the family experience with schizophrenia, but also why it can be such a long and difficult process to change the legal barriers to getting our loved ones the help they so desperately need (but think they don't).
When I wrote Ben Behind His Voices almost ten (!!) years ago, there were very few memoirs about the family experience with schizophrenia- and even few that offered any hope or action steps. Since then, I've seen (and read) quite a few - and this one stands out for its honesty, its perspective (Mindy is the granddaughter of, as well as mother of, someone with schizophrenia), and its knowledge about advocacy and the way things work in the world of state legislation.
Mindy Greiling is a fine writer - you'll keep turning the pages. You'll feel less alone, if you share this issue. And you'll get a really accurate ride on the roller coaster of family experience with "recovery" - what happens after someone with severe mental illness is treated and released? I know this ride all too well - am on it right now, as my son Ben is nearing the end of a three-month hospitalization after nine years of relative success.
Highly recommended.
Can I Divorce My Child? : How Schizophrenia Splits Families Apart
how - and when - do you let go?
Another hospitalization for Ben, another crisis.
Another round of uncovering the truths behind the life he’d sworn he was managing well (“it’s none of your business, Mom”). In the five weeks since this latest breakdown, I’ve been unraveling and trying to piece together the strands of the web he’d woven, and all that was caught in it: the mess, the mounting debt, his addiction to marijuana, the car damage, the shopping sprees, the lies.
I am not legally responsible for any of this, but of course I am a mother and each day includes hours of work to talk with Social Security, Medicare, debt collectors, lawyers, banks. I am doing what I can to prevent the final collapse of the life he’d struggled - with adolescent (at best) decision making, to create, the nine years he has lived with us (no rent) and complied with our requirement that he take his meds.
Our nest was supposed to be blissfully empty by now. My husband and I have more than earned it. But this is my child…the baby I birthed and nursed, the child who was always so impatient to give you a present, the big brother who was such a role model and friend to his sister, the student who was a John Hopkins scholar in eighth grade.
How much do you let go before the guilt chokes you? I think I know now. Ben cannot live with us anymore, if he ever gets back to the “almost normal” he had before he took himself off meds. I must turn him over, once again, to “the system” – because I can’t endanger the rest of my family, or my own sanity, anymore.
But how can I divorce my child? Can any parent do that?
Another day, another new book about the toll when schizophrenia strikes the child you love so much. This one is called Fix What You Can: Schizophrenia and a Lawmaker's Fight for Her Son; I will read and review in a later post, but for now let me say that the reviews are stellar, and the twist is that the author Mindy Greiling is also a former legislator in Minnesota whose advocacy has taken the form of changing mental health laws in that state.
I am always a little bit jealous when a new book is released. Mine continues to sell, but still I envy the excitement of a new memoir – the attention, the possibility, the initial sales. It’s a bit like the feeling when your friend welcomes a new baby - this child could grow up to be a Nobel Prize winner! A famous movie star! The President! – before the messiness of actual life comes in and the blank pages of that child’s life get filled in with actual reality.
But my jealousy right now is more about motherhood than authorship. According to the StarTribune in Minnesota, the author’s son, Jim Greiling,
“ … has passed his 40th birthday because his parents and older sister have been steadfastly behind him, providing emotional, physical and financial support through crisis after crisis. Through suicide attempts, incarceration, chemical dependency relapses, debilitating pharmacological side effects and more, Jim was never alone.”
That was my Ben, too –my 38-year-old son who was working full-time, managing much of his own life (but not his medication), and living with his family – until August 29th of this year.
That’s when it all came tumbling down. Ben was hospitalized for the ninth time – and he is still there. I shared this story in an earlier post, but the update is:
He has been court ordered to take meds but is still finding ways to “cheek” them and still talks only to his voices in the hospital (unless he needs toilet paper or something)
He doesn’t want to see me because he is suspicious of me, and not even sure I am his mother.
The secrets he kept, the lies he told, the damage and debt he covered up, the evidence of drug use…it all keeps adding up, beyond stress, to the dangerousness of his living with us anymore – no matter how much I love him.
What will happen to him next? How will he feel when/if he finally returns to “reality” to find that he has lost his credit rating, his car, his work (well, Covid-19 was to blame for that) – and, now, the security of living in a nice house in the suburbs with the family that loves him?
Back to a state-run (if we can even manage that) group home? This man who, before Covid economy, was working full time as a restaurant server, earning positive yelp reviews for his service and charm?
He worked so hard. But his main goal in life now is to NOT TAKE MEDS. And that breaks my heart. I am powerless to help him.
How can I divorce my child? Do I endanger myself and the rest of the family to keep a roof over the head of someone who hates me, who undermines me, who might possibly start a fire in the house when using the blow torch we found in his room?
Guilt, shame, reality, hope, love, helplessness, grief…I feel it all, for him and for all of us – my family, all the families who face this in a never-ending cycle of confusion and waiting for the other shoe to drop.
Mindy Grelling’s’ advocacy work took the form of legislation. Mine takes the form of education (I teach, and train others to teach, NAMI’s Family-to-Family class; I do public speaking share our story and advocate for change). We both are authors, and we both are devoted mothers.
But that delicate balance…stepping in vs. letting go. That is the hardest part.
For now, I’ll call my decision a legal separation from Ben. We never lose hope. But boundaries must be set, for there are many in our family whose emotional and physical safety must be considered.
I hate schizophrenia so much.
Guilt, shame, reality, hope, love, helplessness, grief…I feel it all, for him and for all of us – my family, all the families who face this in a never-ending cycle of confusion and waiting for the other shoe to drop.